When comparing findings on data quality, maternal characteristics and measures between the two reporting years, our findings have remained generally stable and many findings were similar to the previous report both at national and at trust/board level. Where changes are seen, it should be noted that these are changes only over two discrete periods in time, and therefore cannot be considered to be trends at this stage. Recommendations from the NMPA report on 2015/16 data remain relevant, particularly those related to data quality and to the wide variation in rates of smoking cessation, breastfeeding and skin-to-skin contact. All users of this report should review and assess their performance locally against data in this report and consider improvement action required in response. (All users of this report) |  |
The quality and completeness of data submitted to the NMPA has improved between the 2015/16 and 2016/17 reporting years; however, many trusts and boards are still excluded from one or more measures owing to poor data quality and completeness. Maternity service providers and national organisations responsible for collating and managing maternity datasets should use the NMPA data items described in the NMPA Measures Technical Specification as a guide to focus improvements to data quality. (National organisations responsible for collating and managing maternity datasets, maternity service providers) |  |
There is variation between and within the three countries in the availability, quality and completeness of the data items used to generate the measures in this report. National organisations from across England, Wales and Scotland that are responsible for collating and managing maternity datasets should work together to ensure alignment of data specifications used. (National organisations responsible for collating and managing maternity datasets, with support and input from maternity service providers and from national governments and NHS bodies) |  |
Only a minority of trusts and boards submitted data of sufficient completeness and quality to be included in the measure of birth without intervention. The quality of data collected about smoking in pregnancy and at the time of birth is poor. This is concerning given the importance of smoking cessation as part of initiatives to reduce stillbirth. The quality and completeness of the data items needed to determine place of birth, in particular where obstetric units and alongside midwifery units are co-located, remains variable. Where local data provided have been insufficient to report results, or where results suggest there may be data quality issues for any or all of the following measures:
• birth without intervention
• smoking in pregnancy
• planned and actual place of birth,
maternity service providers should work with maternity information system suppliers and those responsible for collating and managing maternity datasets to improve completeness and accuracy of the data items required for these measures to inform local quality improvement activities. (Maternity service providers, national organisations responsible for collating and managing maternity datasets, maternity information system suppliers) |  |
More than half (50.4%) of women with a recorded BMI at booking were overweight or obese (up from 47.3% in 2015/16). Maternity services, primary care and public health services should work together, with involvement of local service users, to ensure that there is appropriate provision to support weight management prior to, during and after pregnancy (Maternity service providers, public health service providers, commissioners, primary care, women and their families and organisations representing service users) |  |
There is a small increase in induction rates (27.9% to 29.2%) and a small decrease in the proportion of small-for-gestational-age babies born at or after 40 weeks (55.3% to 52.3%) in England only compared with 2015/16 data. This coincides with the introduction of the Saving Babies’ Lives care bundle and requires further monitoring. The NMPA, MBRRACE-UK and other national organisations responsible for collating and managing maternity datasets should continue to monitor for evidence of improvements in:
• the rate of detection of small-for-gestational-age babies
• stillbirth rates (NMPA, MBRRACE-UK and national organisations responsible for collating and managing maternity datasets) Following implementation of national initiatives such as the Saving Babies’ Lives care bundle in England, the NMPA and NHS trusts and boards should monitor for possible increases in induction rates and the impact of this on women, their babies and service providers. (NMPA, NHS trusts and boards) | 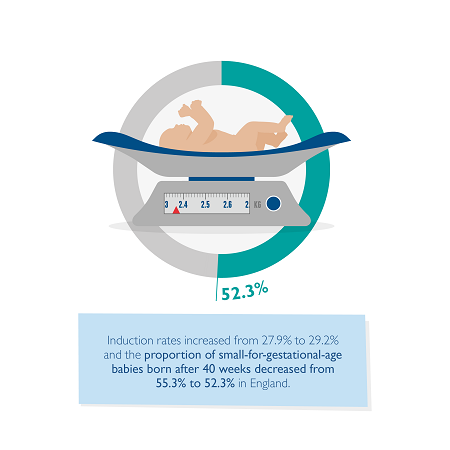 |
There remains substantial variation, beyond that which would be expected due to chance, in the rates of key measures of maternity care such as induction of labour and modes of birth. This suggests that there remains variation in clinical practice, decision making and outcomes across England, Scotland and Wales. National bodies such as NHS England, the Scottish Government, the Welsh Government, the RCOG and the RCM should work together to review the need for guidance and standards to reduce variation in key aspects of maternity care, including induction of labour and modes of birth. (National bodies including the RCOG, RCM, NICE and SIGN, all clinicians, women and their families and organisations representing service users) |  |
Among the 163 508 women with singleton pregnancies who gave birth at term for whom available data were of sufficient quality, 36.9% did so without intervention (spontaneous onset, progress and birth, without epidural, spinal or general anaesthesia and without episiotomy). There was substantial variation in this rate (between 23% and 48%), which persisted after adjustment for case mix. Maternity service providers and local service users should work together to understand the barriers to birth without intervention in their service by reviewing:
• rates of birth without intervention (where local data provided have been adequate to report against this measure)
• rates of individual interventions
• place of birth. (Trusts and boards, women and their families and organisations representing service users) | 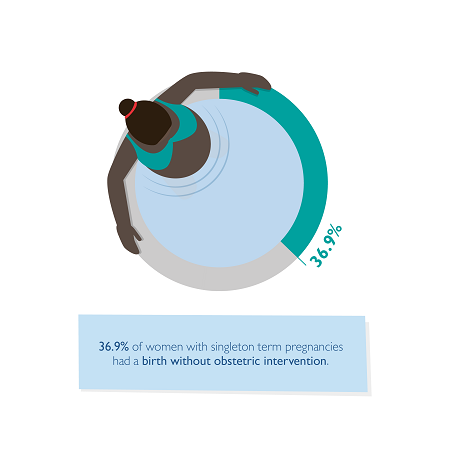 |
There remains variation, beyond that which would be expected, in the proportion of women experiencing complications at birth in the form of a third or fourth degree tear, or a postpartum haemorrhage of 1500 ml or more. National bodies should continue their work to develop and implement package interventions for prevention and management of third and fourth degree tears and postpartum haemorrhage. (National bodies including the RCOG and RCM, and national governments and NHS bodies) All maternity services should review their clinical practices to ensure an accurate diagnosis and effective prevention and management of:
• postpartum haemorrhage
• obstetric anal sphincter injury
to minimise variations in care. (Maternity service providers) | 
|
5.8% of babies born between 37+0 and 42+6 weeks of gestation (term), and 41.9% of those born between 34+0 and 36+6 weeks (late preterm), are admitted to a neonatal unit. There is substantial variation in these rates, even after adjustment for maternal case mix factors, perhaps reflecting different organisational provision for babies requiring additional care after birth. Maternity and neonatal service providers should together review their rates of late preterm and term admissions to neonatal units and consider whether any of their admissions may be avoidable. The NMPA endorses the recommendations made by the ATAIN programme to address avoidable term admissions. (Maternity and neonatal service providers) |  |
5.8 in 1000 babies born between 37+0 and 42+6 weeks of gestation receive mechanical ventilation in the first 3 days of life. There are a number of trusts and boards with levels of ventilation that are higher than expected, even after adjustment for maternal case mix factors. Maternity and neonatal service providers with higher than expected levels of mechanical ventilation between 37+0 and 42+6 weeks should work together to explore reasons behind the variation and implement any changes to clinical practice identified. (Maternity and neonatal service providers) | 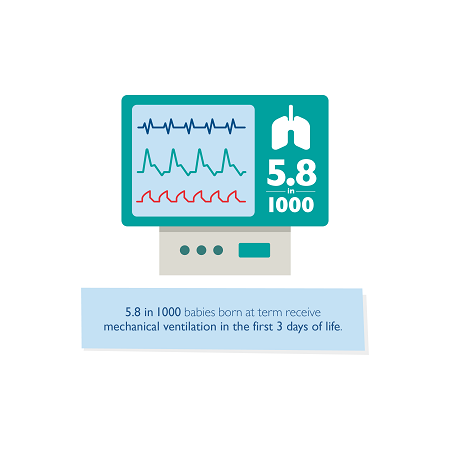 |
1.7 in 1000 babies born between 35+0 and 42+6 weeks of gestation develop an encephalopathy, a component of neonatal brain injury, in the first 3 days of life. Following adjustment for case mix, there are a number of trusts and boards with higher levels of encephalopathy than expected. Maternity and neonatal service providers with higher than expected rates of encephalopathy between 35+0 and 42+6 weeks should work together to explore reasons behind the variation and implement any identified actions and changes to clinical practice. (Maternity and neonatal service providers) National projects working in the area of neonatal brain injury (NNAP, NMPA, Each Baby Counts) should work together to develop an agreed, jointly used, measurable definition for neonatal encephalopathy as a component of neonatal brain injury to ensure consistent measurement. (NMPA, NNAP, Each Baby Counts, Healthcare Safety Investigation Branch, other national projects) | 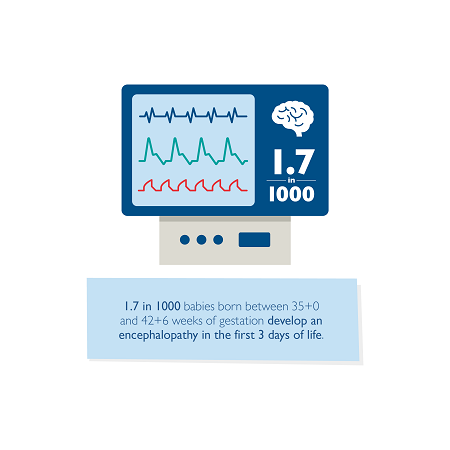 |